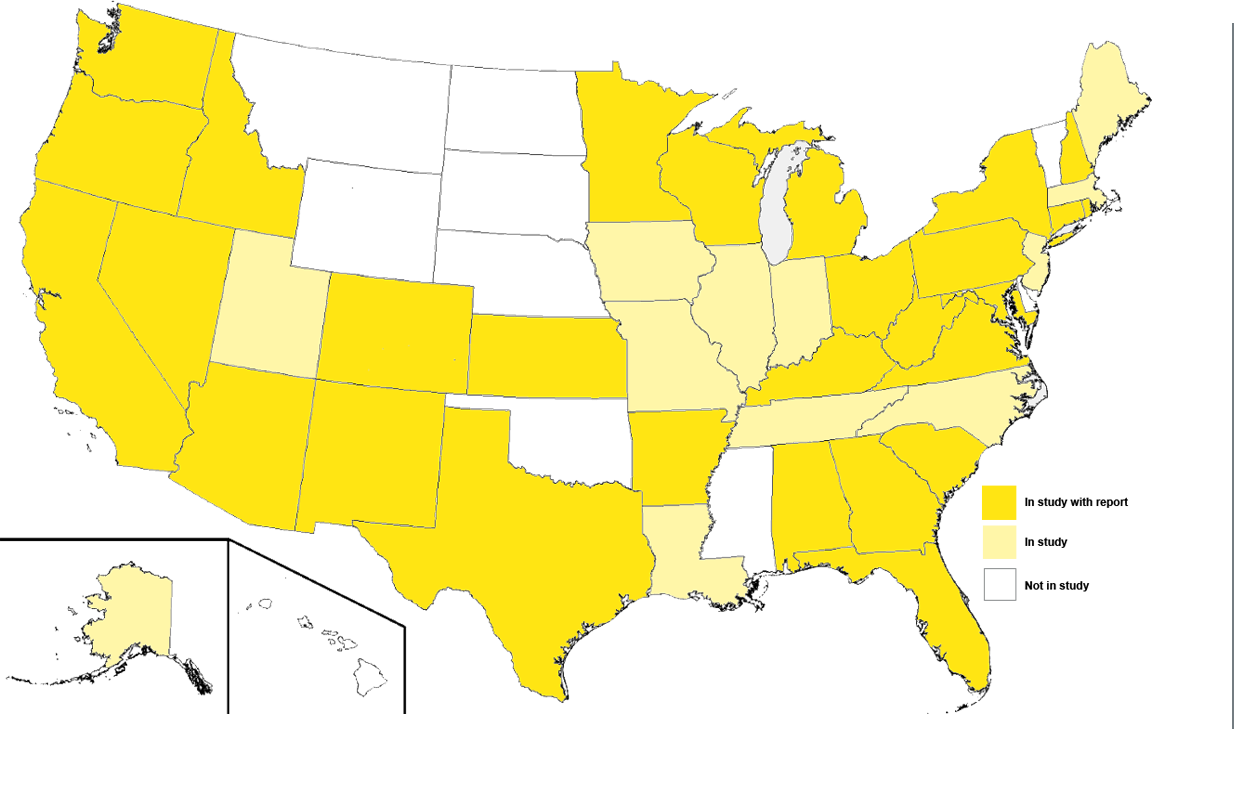
Our collaborative Affordable Care Act Implementation Network connects researchers across the country to follow and analyze the implementation of this broad and quickly evolving law.
Learn more and read the reports.

This brief explores emerging models of care for individuals with complex medical, behavioral, and social needs.
View Report